Bilirubin is a key component of bile, produced in the liver, spleen, and bone marrow. It arises from the breakdown of hemoglobin during the destruction of red blood cells. Bilirubin is an important indicator of liver health and overall bodily function. The bilirubin test offers valuable insights into medical issues such as jaundice, liver diseases, and bile duct obstructions. By grasping its significance, production process, and different types, healthcare professionals can effectively diagnose and manage a range of health conditions. Here’s everything you need to know about bilirubin and what your test results might mean.
What is Bilirubin and Why is it Important?
The Role of Bilirubin in the Body
Bilirubin is a yellow substance produced when red blood cells break down. The liver processes it, and it is then excreted in bile. This function is crucial for removing old cells and toxins from the bloodstream. Maintaining healthy bilirubin levels is vital for overall health, as they reflect proper liver function.
Types of Bilirubin: Direct vs. Indirect
Bilirubin comes in three forms: total, direct (conjugated), and indirect (unconjugated).
1. Total Bilirubin
otal bilirubin is the sum of direct and indirect bilirubin. When jaundice occurs, the total bilirubin level rises.
2. Direct or Conjugated Bilirubin
Typically, direct or conjugated bilirubin is eliminated through the gastrointestinal (GI) tract, with only small amounts entering the bloodstream. It was named “direct” bilirubin because this water-soluble form reacts directly with the reagents used in blood tests. Its levels increase in the blood during obstructive jaundice (such as from gallstones) or hepatic jaundice, as bilirubin cannot reach the intestines for excretion and instead enters the bloodstream to be filtered by the kidneys. Direct bilirubin is the only type that can pass through the glomerular filter, making it the only form detectable in urine.
3. Indirect, Free or Unconjugated Bilirubin
Indirect bilirubin, also referred to as free or unconjugated bilirubin, is typically found in the bloodstream. Its name reflects the fact that this non-water-soluble bilirubin does not react directly with blood sample reagents; alcohol must be added for a reaction to occur. Indirect bilirubin levels rise in cases of hemolytic jaundice, where the breakdown of hemoglobin leads to increased levels of indirect bilirubin in the bloodstream. This type is also elevated in conditions like hepatocellular dysfunction, such as hepatitis. Usually, only the total bilirubin level is reported, and if it is abnormal, further tests are conducted to distinguish between direct and indirect bilirubin levels.
Production of Bilirubin
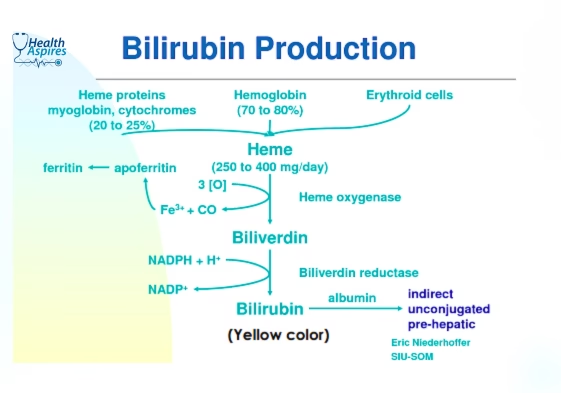
Bilirubin is a substance produced when red blood cells (RBCs) and other heme-containing proteins break down. The process of bilirubin production involves several steps, including:
- Breakdown of RBCs: In the spleen, hemoglobin from RBCs is broken down, releasing heme, iron, and protein.
- Heme oxygenase: The enzyme heme oxygenase acts on the heme ring, producing biliverdin, carbon monoxide, and iron.
- Biliverdin reductase: The enzyme biliverdin reductase converts biliverdin into bilirubin.
- Liver processing: The liver processes bilirubin along with other waste products to create bile.
- Bile delivery: Bile that contains bilirubin is then transported to the intestine.
Sources of bilirubin
- RBCs: Approximately 80% of bilirubin is generated from the breakdown of hemoglobin in aging and prematurely destroyed RBCs.
- Other heme-containing proteins: The remaining 20% of bilirubin is derived from the breakdown of heme-containing proteins found in other tissues, such as the liver and muscles.
Why Does Bilirubin Get Tested?
Bilirubin testing is essential for diagnosing and monitoring issues related to liver function and the breakdown of red blood cells. It is particularly important for identifying:
- Liver Diseases: Such as hepatitis, cirrhosis, and alcoholic liver disease.
- Hemolytic Disorders: Conditions that lead to excessive breakdown of red blood cells.
- Bile Duct Obstructions: Including gallstones or tumors that impact bile flow.
- Neonatal Jaundice: A common condition in newborns that requires immediate attention.
Initial assessments should clarify whether the elevated serum bilirubin is conjugated (direct) or unconjugated (indirect). Asymptomatic adult patients with mild isolated unconjugated hyperbilirubinemia should be evaluated for Gilbert’s syndrome, hemolysis, and medication-induced hyperbilirubinemia. If conjugated hyperbilirubinemia is detected, it is important to check for any accompanying elevations in alkaline phosphatase (ALP) and S.G.P.T (ALT) Test Alanine Aminotransferase and rule out biliary obstruction.
When Should You Get a Bilirubin Test?
A bilirubin test is usually ordered in the following situations:
- Symptoms of Jaundice: This includes yellowing of the skin and eyes, dark urine, and pale stools.
- Monitoring Liver Function: Particularly in patients with a history of liver diseases or conditions that may affect liver health.
- Suspected Hemolysis: Signs like unexplained fatigue, shortness of breath, or dark urine may indicate red blood cell breakdown.
- Routine Newborn Screening: To check bilirubin levels and prevent complications associated with neonatal jaundice.
How is a Bilirubin Test Performed?
Test Preparation: What You Need to Know
Typically, no special preparation is required before the test. but Adequate preparation ensures accurate test results:
- Fasting: Do not eat or drink anything (other than water) for 4 to 6 hours before the test.
- Medication Review: Let your healthcare provider know about any medications you are taking, as some may affect bilirubin levels.
- Alcohol Abstinence: Avoid alcohol for at least 24 hours before the test.
Blood Sample Collection Process
A 3-mL blood sample is drawn in a lavender-top collection tube. A healthcare provider will clean a spot on your arm and insert a needle to collect a vial of blood. The whole process is quick and usually takes just a few minutes. For new born a small amount of blood can taken from the heel (heel prick).
Post Blood Sample Collection
- Apply pressure to the venipuncture site and place a dressing, checking periodically for any bleeding.
- Protect the specimen from bright light by wrapping the sample tube in foil or storing it in a refrigerator.
- Label the specimen and send it to the laboratory.
- Report any abnormal findings to the primary care provider.
Normal Ranges/ Values of Bilirubin
| mg/dL | mol/L | |
| Total bilirubin | 0.3 – 1.0 | 5 – 17 |
| Direct (conjugated) bilirubin | 0.0 – 0.4 | 0 – 7 |
| Indirect (unconjugated) bilirubin | 0.1 – 1.0 | 1 – 17 |
Clinical Interpretation of the Bilirubin Test
Elevated Total Bilirubin
An increase in total bilirubin levels can indicate possible liver dysfunction, hemolysis, or bile duct obstruction. A thorough assessment of both direct and indirect bilirubin levels is essential for diagnosing the underlying issue.
High Indirect Bilirubin
Common Causes:
- o Hemolysis from conditions such as autoimmune hemolytic anemia or malaria.
- o Gilbert’s syndrome or Crigler-Najjar syndrome.
- o Ineffective bilirubin conjugation by the liver.
Symptoms: Fatigue, dark urine, and mild jaundice.
High Direct Bilirubin
Common Causes:
- o Obstructive jaundice due to gallstones or tumors.
- o Liver damage from hepatitis or cirrhosis.
- o Cholestasis resulting from intrahepatic or extrahepatic bile flow problems.
Symptoms: Severe jaundice, abdominal pain, nausea, and pale stools.
Neonatal Bilirubin
- Physiological Jaundice: A frequent condition in newborns that typically resolves as the liver develops.
- Pathological Jaundice: May signal hemolysis, infections, or metabolic disorders and needs prompt medical evaluation.
Possible Meanings of Abnormal Values
| Increased Direct (Conjugated) Bilirubin | Increased Indirect (Unconjugated) Bilirubin |
| Biliary obstruction Cancer of the head of the pancreas Choledocholithiasis Cirrhosis Dubin-Johnson syndrome Hepatitis Obstructive jaundice Pregnancy | Autoimmune hemolysis Cirrhosis Crigler-Najjer syndrome Erythroblastosis fetalis Gilbert’s syndrome Hemolytic transfusion reaction Hepatitis Malaria Myocardial infarction Pernicious anemia Septicemia Sickle cell disease Tissue hemorrhage |
Factors Contributing to Abnormal Values
- Test results can be affected if the blood sample is hemolyzed.
- If a blood sample is exposed to sunlight or artificial light for an hour or more, the bilirubin concentration will decrease.
- Testing with contrast media within 24 hours can alter test results.
- Medications such as allopurinol, anabolic steroids, antimalarials, ascorbic acid, azathioprine, chlorpropamide, cholinergics, codeine, dextran, diuretics, adrenaline, isoproterenol, levodopa, MAO inhibitors, meperidine, methyldopa, methotrexate, morphine, oral contraceptives, phenazopyridine, phenothiazines, quinidine, rifampin, streptomycin, theophylline, tyrosine, and vitamin A may increase total bilirubin levels.
- Conversely, barbiturates, caffeine, chlorine, citrate, corticosteroids, ethanol, penicillin, protein, salicylates, sulfonamides, and urea can potentially lower total bilirubin.
How to Managing High Bilirubin Levels?
Lifestyle Changes for Liver Health
To support liver health and keep bilirubin levels in check, consider the following:
- Consuming a balanced diet that includes plenty of fruits, vegetables, and whole grains
- Reducing alcohol consumption
- Engaging in regular physical activity
- Maintaining a healthy body weight
Medical Treatments for High Bilirubin
If bilirubin levels remain elevated, medical interventions may involve medications to treat the underlying issue. In more serious cases, procedures to eliminate blockages or even liver transplants might be required.
Importance of Regular Follow-Up
Routine check-ups are essential for monitoring bilirubin levels and liver function, allowing for prompt action if needed.
Common Questions and Answers
Q1. What does high bilirubin indicate?
Ans. High bilirubin levels can indicate liver disease, hemolysis, or an obstruction in the bile duct. A detailed evaluation of both direct and indirect bilirubin levels is essential to identify the specific cause.
Q2: How can I reduce elevated bilirubin levels?
Ans. To lower elevated bilirubin levels, it’s important to treat the underlying issue, stay well-hydrated, and steer clear of alcohol or drugs that can harm the liver.
Q3. When Should I Get my Bilirubin Test?
Ans. You should consider getting a bilirubin test if you experience:
- Yellowing of the skin and eyes (jaundice).
- Dark urine and light-colored stools.
- Pain in the abdomen, particularly in the upper right side.
- Feelings of nausea, vomiting, and overall tiredness.
- Itchy skin, often seen in conditions that lead to bile accumulation.
Q4. What is Jaundice?
Ans. Jaundice is a medical condition that leads to a yellowing of the skin, the whites of the eyes, and mucous membranes. This yellow hue results from a buildup of bilirubin, which is a byproduct formed when the body breaks down old red blood cells.
Q5. what is neonatal jaundice?
Ans. Neonatal jaundice is marked by a yellowing of a newborn’s skin and eyes, caused by a buildup of bilirubin in the bloodstream. Bilirubin is a yellow pigment produced when red blood cells are broken down. This condition is quite common in newborns because their underdeveloped livers may have difficulty processing bilirubin effectively.
Q5. Can high bilirubin levels be life-threatening?
Ans. High bilirubin levels are not immediately life-threatening, but they can signal serious underlying health issues like liver disease, gallstones, or jaundice, which can pose significant health risks. Thus, while bilirubin serves as a marker for potential problems, it is crucial to explore the underlying cause and tackle any serious conditions that may exist.
Q7. Can diet influence bilirubin levels?
Ans. Diet can indeed affect bilirubin levels. Research indicates that eating fruits and vegetables rich in flavonoids might raise bilirubin levels, whereas a high-fat diet could lead to lower total serum bilirubin, possibly because of increased caloric intake. Furthermore, an individual’s diet is vital for both the recovery from and prevention of jaundice, underscoring the significance of diet for maintaining liver health.
Q8. What is Gilbert’s syndrome?
Ans. Gilbert’s syndrome is a prevalent and typically benign genetic liver disorder where the liver struggles to effectively process bilirubin, leading to mildly elevated bilirubin levels in the bloodstream. While this can cause symptoms like jaundice, many people with the condition do not experience any noticeable symptoms.
Q9. How does bilirubin affect newborns?
Ans. Bilirubin impacts newborns mainly by leading to jaundice, which is marked by a yellowing of the skin and eyes. This happens because of an accumulation of bilirubin in the baby’s bloodstream, commonly observed in the initial days after birth. Elevated bilirubin levels can result in dehydration and reduced urination; if not addressed, it may necessitate medical intervention.
Q10. What foods to avoid with high bilirubin levels?
Ans. If you have high bilirubin levels, it’s best to steer clear of certain foods that can harm liver function. Key items to limit include:
- Fried foods and those high in fat
- Sugary snacks and refined carbs
- Alcohol
- Highly processed foods
Moreover, it’s wise to avoid unpasteurized products like dairy or fruit juice to reduce the risk of foodborne illnesses that could further strain the liver. Focusing on a diet that supports liver health and encourages hydration during recovery is essential.
