What is Hemophilia?
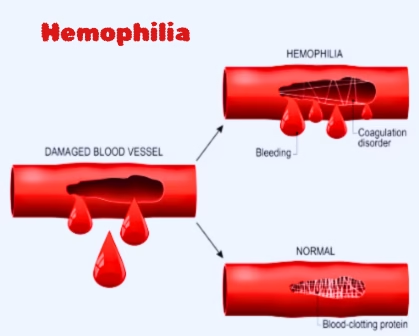
Hemophilia is a genetic bleeding disorder marked by the blood’s inability to clot adequately. This issue arises from either a deficiency or dysfunction of certain clotting factors, which are proteins vital for the coagulation of blood. Consequently, those with disease may experience prolong bleeding, both on the externally and internally within the body, even from minor injuries.
Hemophilia mainly impacts males because it is an X-linked recessive condition. While females frequently carry the gene, they rarely show symptoms. The condition’s severity can differ based on the activity level of clotting factors present in the blood.
Causes of Hemophilia
Hemophilia results from mutations in the genes that encode clotting factors. The two most prevalent types of hemophilia are:
- Hemophilia A: This type arises from a shortage of clotting factor VIII (FVIII) and is the most common form, making up roughly 80% of all cases.
- Hemophilia B: This type results from a lack of clotting factor IX (FIX) and is less frequent, often referred to as “Christmas disease.”
- Hemophilia C: Genetic mutation in clotting factor genes present on Chromosome 4 which is inherited in autosomal recessive pattern.
These mutations follow an X-linked recessive inheritance pattern. Males possess only one X chromosome, so a single mutated gene can lead to the disorder. In contrast, females have two X chromosomes and typically act as carriers unless both X chromosomes are mutated, which is uncommon.
Approximately 30% of hemophilia cases result from spontaneous mutations with no prior family history of the disorder, known as de novo mutation.
Signs and symptoms of Hemophilia

- Bruising
- Hematomas, which is when there is bleeding into the muscle or soft tissues
- Bleeding from the mouth and gums
- Bleeding after a circumcision
- Blood in the stool
- Blood in the urine
- Nosebleeds that are frequent and difficult to stop
- Bleeding after vaccinations or other injections
- Bleeding into the joints
Complications of Hemophilia:
- Joint damage
- Muscle hematomas
- Chronic Anemia
- Risk of infections
- Excessive bleeding during surgery
- Adverse effect to treatment
How To Avoid Complications of Hemophilia ?
- Avoid injury
- Avoid IM injections
- Immunization against hepatitis B
- Providing emotional support
- Precautions before surgery
Types of Hemophilia
The primary types of hemophilia include:
Hemophilia A (Classic Hemophilia):
- This is caused by a lack or deficiency of clotting factor VIII.
- It is the most prevalent form, representing approximately 80% of cases.
- The severity varies based on the level of factor VIII activity:
- Mild: 5-40% of the normal factor VIII activity.
- Moderate: 1-5% of the normal factor VIII activity.
- Severe: Less than 1% of the normal factor VIII activity.
Hemophilia B (Christmas Disease):
- This condition arises from a deficiency or absence of clotting factor IX.
- It is less common than Hemophilia A, comprising about 20% of cases.
- The severity is also categorized as mild, moderate, or severe, depending on the level of factor IX activity.
Hemophilia C
- This is due to a deficiency of clotting factor XI.
- It is much less common than Hemophilia A and B.
- Symptoms are generally milder and are mainly observed in Ashkenazi Jewish populations.
Acquired Hemophilia:
- This is an uncommon autoimmune disorder where the body produces antibodies against its own clotting factors (typically factor VIII).
- It is not inherited and can arise in individuals without a family history of hemophilia.
Hemophilia A and B are X-linked recessive conditions, meaning they mainly affect males, while females are generally carriers. Hemophilia C is inherited in an autosomal recessive manner and can affect both males and females equally.
Classification of Hemophilia on the base of Clotting factor activity
Hemophilia is categorized according to the severity of the disorder, which is evaluated by the level of clotting factor activity present in the blood:
- Mild Hemophilia:
- Clotting factor activity: 5–40% of the normal level.
- Symptoms: Extended bleeding following surgical procedures, dental work, or significant injuries. Spontaneous bleeding is uncommon.
- Moderate Hemophilia:
- Clotting factor activity: 1–5% of the normal level.
- Symptoms: Bleeding occurs after minor injuries or surgical interventions. There may be occasional spontaneous bleeding.
- Severe Hemophilia:
- Clotting factor activity: Less than 1% of the normal level.
- Symptoms: Regular spontaneous bleeding into joints, muscles, and internal organs. Bleeding can happen without any obvious reason.
Epidemiology of Hemophilia
Hemophilia is an uncommon condition, though its occurrence differs among different populations. Current research estimates
- The global incidence of hemophilia A at 1 in 10,000 births and hemophilia B at 1 in 50,000 births.
- Around 400,000 individuals worldwide have hemophilia, with roughly 20,000 residing in the United States.
- Hemophilia A is approximately four times more prevalent than hemophilia B.
- Improvements in treatment have greatly enhanced life expectancy, allowing many patients to live into their 60s and even longer.
Diagnosis of Hemophilia
Early diagnosis of hemophilia is essential for effective treatment and avoidance of complications. The diagnostic procedure consists of the following steps:
- Clinical Assessment:
- A thorough medical history, including any family background of bleeding disorders.
- Evaluation of symptoms such as extended bleeding, frequent nosebleeds, or unexplained bruising.
- Laboratory Evaluations:
- Complete Blood Count (CBC): Low HCT and low Hb ( due to prolonged bleeding), including platelet disorders.
- Peripheral blood smear: normocytic normochromic RBCs
- Bleeding Time (BT) and Clotting Time (CT): prolonged
- Clotting Factor Assay: To assess the levels of clotting factors VIII and IX. The assay confirms the factor deficiency, helping to distinguish between mild, moderate, and severe forms of Hemophilia
- Activated Partial Thromboplastin Time (aPTT): A prolonged aPTT indicates a deficiency in clotting factors.
- Genetic Analysis: To identify specific mutations in the F8 or F9 genes. This is especially valuable for carrier tests and prenatal diagnosis.
- Prenatal Analysis:
- For families with a hemophilia history, prenatal testing can be conducted using chorionic villus sampling (CVS) or amniocentesis.
Recent improvements in diagnostic methods, such as next-generation sequencing (NGS), have enhanced the accuracy and speed of genetic evaluation, allowing for earlier and more precise diagnoses.
Recent Research and Advancement in Treatment
Recent investigations have concentrated on enhancing treatment options and gaining insight into the molecular mechanisms associated with hemophilia. Some notable advancements include:
- Gene Therapy:
- Gene therapy has demonstrated potential in offering a possible cure for hemophilia. Clinical trials have shown sustained production of clotting factors in individuals with hemophilia A and B following a single administration of gene therapy.
- Extended Half-Life (EHL) Products:
- Innovative clotting factor concentrates featuring extended half-lives decrease the number of infusions necessary for prophylactic treatment, thereby enhancing the quality of life for patients.
- Non-Factor Replacement Therapies:
- Medications such as emicizumab (Hemlibra) imitate the functionality of factor VIII, presenting an alternative for patients with inhibitors (antibodies that counteract clotting factors).
- Global Registries:
- Worldwide registries are gathering data to gain a deeper understanding of the natural progression of hemophilia and the long-term effects of emerging treatments.
