Haemopoiesis
The blood comprises of a fluid part called plasma which make up to 55% volume and the formed elements called cells which is about 45% of whole blood. The blood cells are of 3 types, which red blood cells (RBC), white blood cells (WBC) and platelets (Plt). WBC (White blood Cells) cells are further divided into two main groups, granulocytes (neutrophils, eosinophils and basophils) and agranulocytes, which are monocytes and lymphocytes. The blood cells are constantly destroyed either by aging or as a result of their functional activities and are exchanged by new cells. There is a fine stability between the degrees of formation and destruction of these blood cells in healthy people. The development of all blood cells is called haemopoiesis. ( Hemo: Blood, Poiesis: Development)
Erythropoiesis: The Process of Red Blood Cell Formation
The process of development, differentiation and maturation of RBCs from primitive stem cells It’s a sub-process of hematopoiesis, regulated by erythropoietin (Epo), which is a cytokine produced by the kidneys. Epo binds to a receptor on erythroid progenitor cells, which stimulates the production of RBCs.
Erythropoiesis: Lecture Slide PPT-PDF
Sites of Hematopoiesis / Erythropoiesis
| Embryonic Stage (0-2 months) | Yolk Sac | Produces primitive erythrocytes (RBCs). |
| Fetal Stage (2-7 months) | Liver | Major site of hematopoiesis; produces RBCs, WBCs, and platelets. |
| Fetal Stage (2-7 months) | Spleen | Assists in hematopoiesis, mainly lymphocyte production |
| Fetal to Adult Transition (7 months onward) | Bone Marrow | Becomes the primary site of blood cell production |
| Birth to Adulthood | Red Bone Marrow (Found in flat bones: sternum, ribs, pelvis, skull, vertebrae, proximal femur & humerus) | Produces all blood cells (RBCs, WBCs, platelets). |
| Lymphatic Organs (Throughout Life) | Spleen, Lymph Nodes, Thymus | Produces lymphocytes and supports immune function |
| Pathological Hematopoiesis (Diseases like myelofibrosis, severe anemia) | Liver, Spleen, Lymph Nodes (Extramedullary Hematopoiesis) | Abnormal sites of blood formation in disease conditions |
Origin of Blood Cells
All blood cells are made from the homogenous primitive cell, which looks like a large lymphocyte and is called a pluripotent or totipotent hemopoietic stem cell. It gives rise to lineage-specific stem cells, termed colony-forming units lymphoid and spleen (CFU-L & CFU-S). These in turn distinguish into more devoted stem cells and progenitor cells that can only differentiate on specific lines. These are also called CFUs. The stem cells maintain their number by self-renewal. When the need arises, a stem cell splits into two. One of the daughter cells replaces the parent cell in the stem cell pool while the other differentiates along the required cell line.
All of this takes place under the influence of certain proteins, which are called hemopoietic growth factors. These comprise interleukins (IL) and colony stimulating factors (CSF), which are secreted by various cells in response to stimuli. Important hemopoietic growth factors include IL-3, GM-CSF, G-CSF, and erythropoietin (Epo).There are certain other proteins that have an inhibitory influence on hemopoiesis. For example, interferon (INF) and tumor necrosis factor (TNF).
Steps in RBC Formation (Erythropoiesis)
In normal marrow, the proerythroblast is the first identifiable cell of the erythroid series. It divides and matures to an RBC through various stages. The process of normoblastic maturation is characterized by the following progressive changes.
- • Decrease in cell size
- • Hemoglobinization
- • Extrusion of the nucleus.
The time for maturation from pronormoblast to mature red cell is about 7 days. Various stages in the development of an RBC are:1.
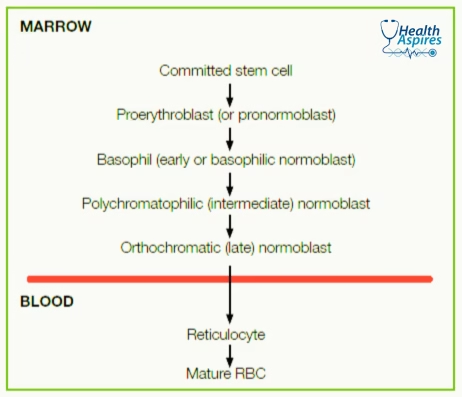
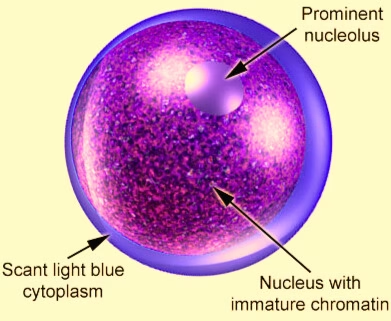
1. Pronormoblast:
It is a round cell with a diameter of 12-20 μm. It has a large nucleus surrounded by a small amount of cytoplasm. The cytoplasm is deep blue in color. The nucleus is round and consists of a network of uniformly distributed chromatin strands. It is reddish purple in color and contains several nucleoli (Plate-I). It divides and matures to basophilic or early normoblast.
2. Basophilic (Early) normoblast:
It is 10-16 μm in diameter. It has a large nucleus with thick chromatin strands and no nucleoli. Cytoplasm is blue like the pronormoblast. It divides and matures into a polychromatic or intermediate normoblast.
3. Polychromatic (intermediate) normoblast:
It is 8-14 μm in diameter. The nucleus occupies a smaller part of the cell and stains deeply. The cytoplasm gives a reddish tinge and is not so blue in color due to the formation of hemoglobin. It divides and matures into orthochromatic or late normoblast.
4. Orthochromatic (Late) normoblast:
It varies from 8 to 10 μm in diameter. The cytoplasm is acidophilic (red) due to hemoglobinization. The nucleus is small and appears as a deeply staining blue-black homogeneous mass (pyknotic). It becomes eccentric in position and is finally extruded out from the cell. Late normoblasts cannot divide and only mature into reticulocytes by extrusion of the nucleus.
5. Reticulocyte:
The reticulocyte is a flat, disc-shaped cell. It has no nucleus and is slightly larger than the mature red cell. It has a diffuse basophilic (bluish) tinge (polychromatic). With supravital stains such as brilliant cresyl blue, the basophilic material, which is RNA, appears in the form of a reticulum. The reticulocyte becomes a mature red cell in about 1-4 days. Half of this time is spent in the spleen.
6. Red Blood Cell (RBC):
The mature RBC is a non-nucleated cell. It is a biconcave disc. It is about 7.2 μm in diameter. The cytoplasm is pink due to the presence of hemoglobin. There is no nucleus, no mitochondria, and no ribosomes.
